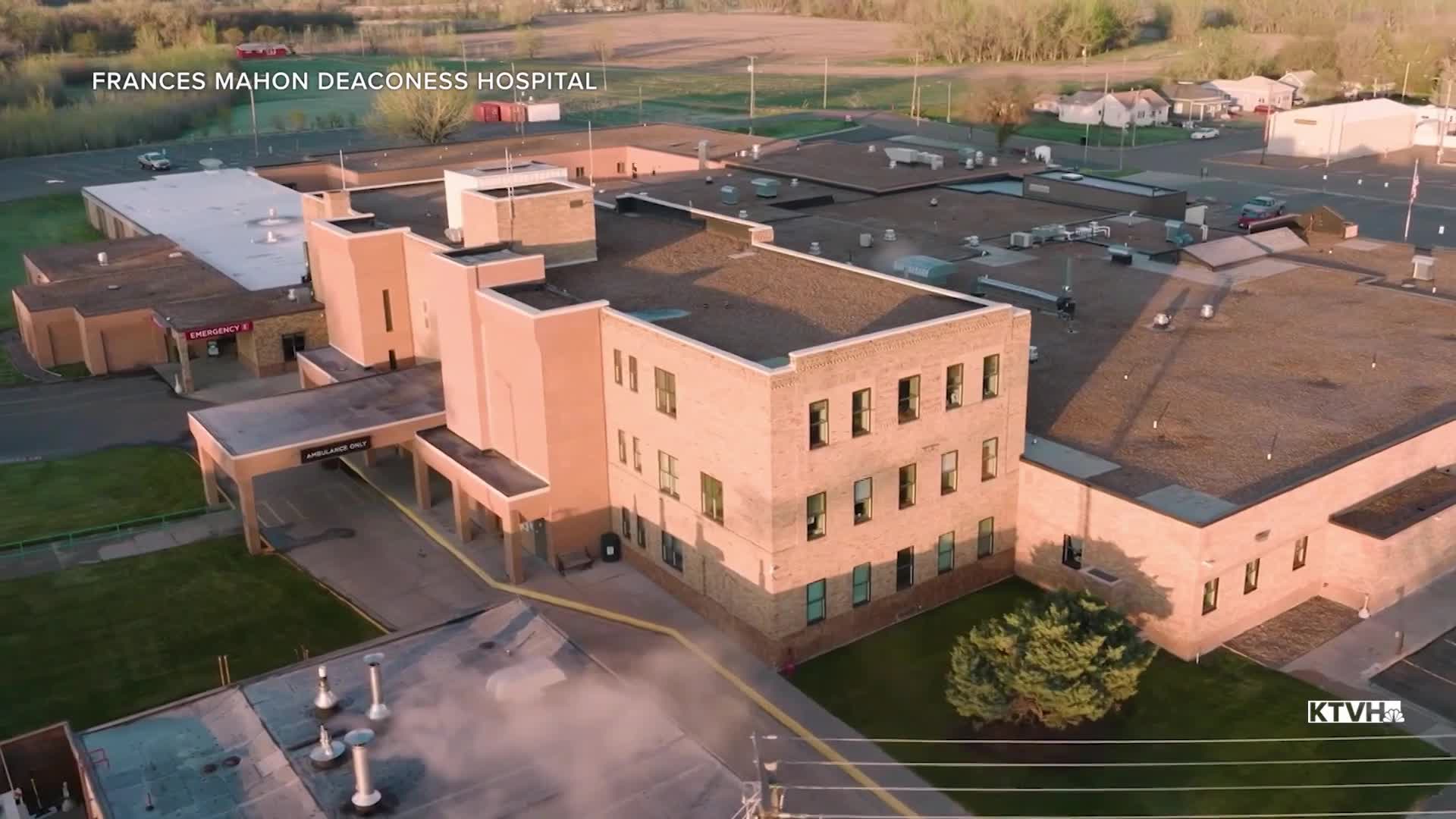
HELENA — Frances Mahon Deaconess Hospital, in Glasgow, serves four counties in northeastern Montana, with around 25,000 people in 14,000 square miles. Leaders say providing health care over a service area like that comes with challenges.
“We’re the most geographically isolated community of at least a thousand people in the contiguous 48 states, and that just creates a lot of challenges with shipping supplies,” said CEO Nick Dirkes.
Dirkes says they’ve also been dealing with issues like an aging population and a smaller available workforce. So when he heard the federal government was proposing to set aside $50 billion to support health care in rural areas, he took notice.
“I think this is a generational opportunity to make meaningful improvements in the way we deliver rural health care,” he said.
HR 1, congressional Republicans’ “One Big Bill” passed last year, created a Rural Health Transformation Program, which will provide each state hundreds of millions of dollars over the next five years. Earlier this week, the federal Centers for Medicare and Medicaid Services announced how much money each state will receive for the first year. Montana was awarded $233.5 million for the 2026 fiscal year – fourth-most of any state, behind only Texas, Alaska and California.
“I think, first, it does speak to the strength and quality of the application that the Gianforte administration submitted,” said Ed Buttrey, president and CEO of the Montana Hospital Association. “Also, I think it has to do with the massive size of the state and the large amount of our population that lives in rural areas. That's where the challenge is, is how do you provide that health care? How do you keep these facilities sustainable?”
The Montana Department of Public Health and Human Services submitted its plan for using the money in November – originally planning, like all states, to receive $200 million per year. The department announced it will put together five initiatives to meet five strategic goals: boosting workforce development and retention, encouraging innovative care models, investing in prevention, expanding use of technology and improving rural providers’ long-term stability.
“I think the application from the state stated that 89% of our rural hospitals have a negative operating margin; this is something that just isn't sustainable over the long term,” Buttrey said. “So we have a tremendous opportunity here to redesign those systems to make sure that they're financially stable, to provide additional enhanced workforce, to look at better ways of coordinating care.”
The RHTP was often positioned in media coverage as a measure to ensure rural hospitals weren’t harmed by the other health care-related changes in HR 1 – most notably, new rules for Medicaid that are expected to significantly reduce federal spending on the program.
Buttrey, who sponsored the renewal of the state’s Medicaid expansion last year in his position as a state representative, said he believes the impacts to Montana providers may not be as big as in other places.
“Montana has a really well-designed system, so we weren't affected as badly as many other states,” he said. “But the idea was, if we're going to cut Medicaid payments and money, the folks that are going to likely struggle the most are going to be your rural health care facilities, so the RHTP is there to make sure that those facilities have an opportunity to redesign themselves, to reimagine, to implement technology.”
DPHHS says it will now revise its planned budget for the program, to account for the additional funding Montana will be receiving. The department says it will host additional stakeholder meetings to keep taking public input on the plan.
Dirkes says he’ll be looking for more details about the specifics of how the state will allocate the money. He says he sees some obvious things they can work on, like expanding the availability of telehealth, partnering on training opportunities and encouraging the use of advanced practice nurses and physician assistants.
Regardless of what ideas come forward, Dirkes says everyone will need to make sure they’re ready to go for the long term.
“We are getting this one-time infusion, but it is one time,” he said. “So whatever we do, we need to be able to sustain it into the future, through either cost savings that we’ve ourselves seen or additional revenue streams. That’s going to be really important.”